Understanding Awake Craniotomy: Why It’s Done and When It’s Preferred
In recent years, brain surgery has evolved to include approaches that focus on both treatment and maintaining brain function. One such advancement is awake craniotomy, a sophisticated neurosurgical procedure that allows surgeons to treat certain brain conditions while the patient is awake and actively participating. This awake procedure is most commonly used to treat conditions near regions of the brain responsible for critical functions.
What is Awake Craniotomy?
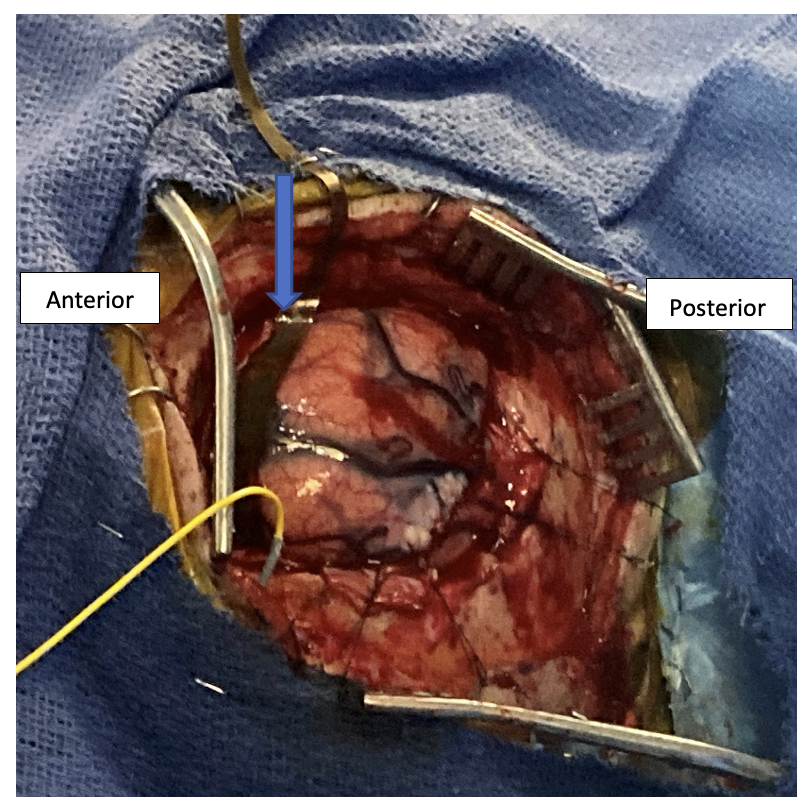
Awake craniotomy, or awake brain surgery, is a type of open brain surgery performed while the patient is conscious during key parts of the procedure. It is typically done using an “asleep-awake-asleep” technique, in which the patient is sedated at the beginning, awakened during the surgery to perform specific tasks, and then sedated again for closure.
This technique is especially useful for treating brain tumors (such as gliomas) or epileptic foci located close to areas of the brain that control essential functions, such as speech, movement, and vision. During the awake phase, the surgeon applies electrical stimulation to different brain regions and observes the patient’s responses, such as moving a limb, naming objects, or reading aloud, to map areas that must be preserved. This mapping helps avoid damage to critical areas during tumor removal.
Depending on the part of the brain being treated, patients may be positioned on their back, side, or even in a sitting posture. The head is held securely with a frame, and the anesthesia team monitors the patient throughout to ensure comfort and responsiveness.
What are the Benefits of Awake Craniotomy?
Awake brain surgery offers several compelling advantages, especially when compared to traditional craniotomies performed under full anesthesia. These include:
- Precise brain mapping: It enables surgeons to locate and avoid critical functional regions.
- Maximized tumor removal: Awake mapping helps remove as much abnormal tissue as possible while preserving healthy brain tissue.
- Better functional outcomes: Patients have a lower risk of postoperative neurological complications like paralysis or speech loss.
- Reduced postoperative pain: Many patients report manageable levels of postoperative pain, often requiring fewer narcotic medications.
- Shorter ICU stays: Patients undergoing awake craniotomy may avoid prolonged ICU stays due to early neurological assessment and fewer complications.
- Improved survival rates: In cases such as low-grade gliomas, maximal safe resection, enabled by awake craniotomy, has been associated with improved survival outcomes.
- Improved seizure control: In patients with epilepsy, it may help significantly reduce or eliminate seizure episodes.
- Functional balance: Surgeons can tailor the extent of tissue removal to balance oncological effectiveness with functional preservation.
What are the Challenges of Awake Craniotomy?
Despite its advantages, awake craniotomy is a highly complex procedure that poses certain intraoperative and postoperative challenges.
During the awake phase, patients may face:
- Mild pain or discomfort, though neuro-anesthesiologists strive to keep patients comfortable.
- Anxiety or fear, which can be alleviated through continuous reassurance from the surgical team.
- Temporary confusion or agitation upon waking from initial sedation. Cooling measures, such as using a cold water-soaked sponge, can offer relief.
- Seizures, although careful stimulation can reduce this risk.
- Nausea and vomiting, managed with appropriate medications.
- Hypertension, commonly observed but controllable with drugs.
After surgery, patients may experience side effects similar to other open brain procedures, including:
- Memory impairment
- Difficulty with speech
- Swelling of the brain
- Muscle weakness
- Meningitis
However, these challenges are often minimized in high-volume centers equipped with modern neurosurgery techniques and a skilled multidisciplinary team. These centers perform comprehensive preoperative assessments to tailor the approach to each patient’s unique needs.
Conclusion
As a specialized surgical approach, awake craniotomy allows surgeons to navigate the brain’s most delicate areas with precision. While not without challenges, its benefits in preserving essential neurological functions make it the preferred option for select patients.